Overcome's Model Explained
This page is written for psychologists, economists, and philanthropists who want to understand the rationale for how we designed our service: the evidence-base, our implementation, and our results so far.
Global Mental Health Crisis

Over 1 billion people worldwide need mental health support, but public spending is insufficient. (See WHO Report)
Traditional face-to-face therapy costs over $1000 per successful treatment (Radhakrishnan et al, 2013). If that was the only approach, the world could only treat ~5% of those who need it.
Despite having 80% of the global population, low and middle-income countries (LMICs) get less than 20% of global mental health funding.
Online Support from
Non-Professionals
After three years of research, we concluded that training non-professionals to deliver online support is the most cost-effective.
Why Online Support?
-
Eliminates venue costs and allows practitioners to work from home, cutting non-salary expenses to nearly zero
-
Systematic reviews show no significant difference on client outcomes compared to face-to-face support (Fernandez et al., 2021)
Why Non-Professionals?
Non-professionals, with a few weeks of training, can deliver effective treatment for depression, anxiety, and other common mental health conditions. This concept is called lay counselling. Multiple systematic reviews and successful interventions across the globe prove that it works.
Systematic Reviews on Lay Counselling
Systematic review of 123 primary studies and 10 meta-analyses concludes that interventions involving lay counselling are effective and should be made routinely available (Barbui et al., 2020).
Systematic review of 1072 studies concludes:
“The use of professionally trained, lay counsellors to provide mental health interventions in low- and middle-income countries was associated with significant improvements in mental health symptoms across a range of settings”
Case Study #1 - Lay counselling for depression (India)
Sangath trained high school graduates to be lay counsellors in three weeks, focusing on behavioural activation (a Cognitive Behavioural Therapy technique). Lay counsellors then provided six to eight support sessions to locals who experienced clinical depression.
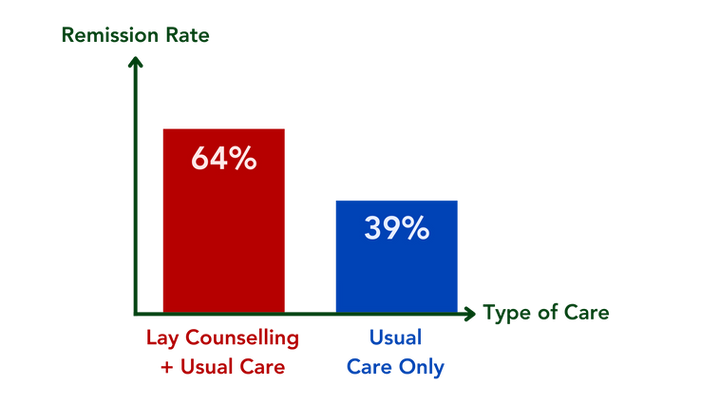
A randomised controlled trial of this intervention showed significantly higher depression remission rates (64%) compared to usual care only (39%; Patel et al., 2017).
Case Study #2 - Lay counselling for depression (Zimbabwe)
Friendship Bench is a community-based model using community volunteers with eight days of training in cognitive behavioural therapy.
A randomised controlled trial showed that the intervention reduced depression prevalence from 50% to 14% (Chibanda et al., 2016). Each treatment costs only ~$3.37 to deliver (Healey et al., 2022)
Case Study #3 - Lay counselling for alcohol problems (India)
After two weeks of classroom training, secondary school graduates with no prior experience to be lay counsellors are given real clients under supervision.
According to a randomised controlled trial, their patients were twice as likely to achieve remission than the control group with no increase in adverse events (Nadkarni et al., 2017). Each remission cost only $217 to achieve (Nadkarni et al., 2017)
Our Approach
We echo the call by the WHO that we need more regular people delivering mental health services, especially for mild-moderate issues.

WHO Guidelines for Mental Health Interventions (WHO, 2023)
“Most psychological interventions may be delivered by a wide range of professional staff: counsellors, psychologists, nurses, lay health counsellors and health volunteers”
“A range of brief psychological treatments including guided/unguided internet-based CBT (iCBT) and [layperson-delivered] psychological treatments were significantly better than treatment as usual (TAU) in reducing depressive symptoms”
Training Aspiring Mental Health Professionals
The case studies above trained those with high school education to deliver the intervention. If high school graduates can make these interventions work, aspiring mental health professionals with psychology degrees can too.
What Aspiring Mental Health Professionals Want
Aspiring mental health professionals told us that:
-
They want to help others across the world.
-
They want to find out if they are suited to the work.
-
They have completed an academic course in psychology, and are disappointed by the lack of focus on the practical skills needed to help others.
-
They need experience that helps them get paid roles, while most opportunities are administrative or shadowing-only.
If there was a dream opportunity that provides them with all of the above, they are willing to volunteer in return for experience, supervision, and training.
Co-Designing the Experience
-
We first trained one person. It worked well, so we scaled up to five.
-
We then tried various modes of training - a mixture of live workshops, role plays, quizzes, and assessments worked best.
-
We learnt together that confidence is one of the biggest barriers. To build up their confidence, they first pass an assessment and start supporting clients with procrastination / diet / exercise. Once they feel comfortable and have passed another assessment, they start seeing clients experiencing low mood / anxiety / fear.
-
At the end of every single cohort, we gather detailed feedback from coaches and use that to improve the experience of the next cohort.
-
As of February 2025, we’re on Cohort 20
Our Training
After two years of iterative improvement, our trainees now receive a four-week intensive training programme before seeing clients.
Week 1 - Motivational Interviewing and Coaching Skills
Helping others execute successfully on behaviour change.
Interpersonal Skills
Fundamental techniques for effective support sessions.
Goal Setting
Strategies to define and achieve personal objectives.
Effective Planning
Methods for organising tasks and reminders efficiently.
Weeks 2 to 3 - Techniques from Evidence-Based Therapies
The 2nd and 3rd week focus on simple but effective techniques from cognitive behavioural therapy and acceptance commitment therapy. Trainees are not trained to deliver a manualised therapy programme, but to integrate these techniques into their coaching.
From cognitive behavioural therapy, we chose techniques for reframing beliefs, emotional regulation and problem-solving. For example, behavioural activation, whose delivery by non-professionals is shown by systematic review (Anvari et al., 2023) to be about as effective as one-to-one therapy with a professional. See below for other examples:
Socratic Questioning
Questioning to challenge and reframe unhelpful thoughts.
Relaxation Techniques
Strategies like progressive muscle relaxation and deep breathing.
Self-Monitoring
Tracking thoughts, emotions, and behaviours to identify patterns.
Complementary techniques from acceptance commitment therapy help people live a life according to their values, set more sensible goals, and react better to things they can’t control. For example:
Clarifying Values
Identifying and prioritising what truly matters to guide decision-making
Acceptance
Allowing thoughts and emotions to exist without judgment.
Defusion
Creating distance from thoughts to reduce their impact on emotions and behaviours.
Week 4 - Guided Self-Help for Phobias and Insomnia
Graded exposure for fear / phobia / social anxiety
Delivery by laypersons is backed by multiple meta-analyses (Cuijpers et al., 2010).
Sleep restriction, sleep hygiene and stimulus control for insomnia
We demonstrated the effectiveness via our randomised feasibility trial and another RCT (Ho et al., 2014) showed similar results. This is unsurprising because even these techniques have been shown to work even with no additional human support given (Tsai et al., 2022). Multiple systematic reviews attest to this (Lin et al., 2023).
Continuous Support for Trainees
Progression is guided by thorough assessments and multiple avenues of support, including:
-
Daily cohort meetings during full-time period where coaches can support each other
-
Weekly internal clinical supervision during full-time period (~Monthly supervision if part-time)
-
One-on-one support from internal clinical supervisor or management team for additional guidance
-
External clinical supervision
-
Internal coaching for any coach who requests it
-
In exceptional circumstances, we can pay for professionally delivered therapy for coaches who need additional support
Seeing Clients
Our trainees become "Mental Health Coaches" after they pass their first assessment. They first start seeing lower-risk clients, such as those working on diet, exercise, procrastination, or similar concerns.
As they gain experience and pass their second assessment, they gradually take on more challenging cases, like low mood, anxious feelings, or fear.
The most experienced coaches may eventually work with clients facing moderate depression, anxiety or phobias.
Coaches are never assigned clients beyond their comfort and confidence level.

Our Intervention
6 x 45-minute one-to-one video call sessions with a coach.
The strongest predictor of client outcomes across conditions is the extent to which the sessions focus on the client's goals, using activities the client believes in (Wampold, 2015).

Therefore, our coaches collaboratively build a plan with the client to tackle the precise issue the client believes is most important. We give our coaches a toolkit of simple but effective techniques derived from proven therapies (e.g., motivational interviewing, cognitive behavioural therapy, acceptance commitment therapy).
For common issues, we provide a default plan coaches and clients can start with, such as:
Behavioural Activation for low mood / depression
Graded exposure for fear / phobia / social anxiety
Sleep restriction, sleep hygiene and stimulus control for insomnia
For topics that our training doesn’t cover directly, the client and the coach co-design an effective plan.
Agree on what topic to work on
Agree on how to work on it
Strong partnership between equals
However, we can't help with issues beyond our abilities:
-
Mental Health Crisis
Immediate risk of self-harm, suicide, or harming others requiring urgent help.
-
Specialist Support
For example, OCD, PTSD, personality disorders, psychosis.
-
Medical Support
Clinical diagnoses, assessments, medications, or certifying evidence.
-
Safeguarding Cases
Active abuse, crimes, or radicalisation that require help from local authorities.
Triaging and Continuous Risk Assessment
Our sign-up form screens out clients seeking help for issues we cannot support with. If clients get passed the screening, but seem less suitable for our programme, our internal clinical supervisor invites them to a meeting where she will discuss their suitability for our programme and signpost them to local services as needed.
If existing clients who have a coach express that they'd like support for issues we cannot help with, these cases get flagged to our internal clinical supervisor / management for further action.
The Evidence
Clients Feel Better and Spread the Word
On average, clients are 2 out of 10 happier after 6 sessions.

They like their sessions, like their coach, and would love to recommend our programme to others. Click here to see the full list of client testimonials.

Our growth from word of mouth has increased drastically in the past 12 months.


Feasibility Trial of our Sleep Programme (n = 36)
The results are comparable to one-to-one cognitive behavioural therapy for insomnia delivered by professionals (Simon et al., 2023).

Our Trainees are Satisfied and Invite Peers
50% of our coaches land jobs to directly deliver mental health interventions after volunteering with us. 67% continued volunteering with us part-time or full-time. Click here to see what our past trainees say about their experience.


Next Steps
Ways to Help More People
Apart from supporting those based in LMICs, we'd like to work out the most impactful demographics to support. For example, supporting charity founders' wellbeing not only affects their individual productivity, but also the beneficiaries of the charities.
Staying Small
Stay small so we can iteratively improve faster:
-
Less bureaucracy
-
Less hierarchy
-
Faster decision making